I
have listened to a public radio program for many years called The Moth Radio
Hour. It is an amazing radio program and now podcasts that can be
downloaded where people tell these amazing real life stories that they have lived
and experienced. One day, I was listening when I heard Mike Birbiglia's amazing
story, which eventually lead to the production of the movie "Sleep Walk
with Me", where Mr. Birbiglia talks about his amazing sleep related
struggles. Here is the link to his story:
Mike Birbiglia "361 Fear of Sleep" -- Moth Radio hour segment
After listening to this incredibly fantastic story, I decided to ask my friend
Richard Smith, who works at WisconsinSleep, which is a sleep clinic in
Madison, as a High Density Sleep Technician as well as for UW-Madison
Dept of Psychiatry in the Center for Sleep andConsciousness as a
Research Specialist, some questions to get a better understanding of sleep,
sleep disorders and it's impact on mental and physical health. Here are the
questions and his responses:
What were your
reactions to Mr. Birbiglia’s humorous but definitely intense story about his
struggles with his sleep disorder?
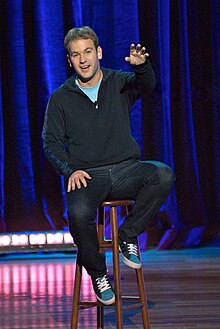 |
| Mike Birbiglia |
What is a REM sleep
disorder?
Rapid Eye Movement (REM) Sleep Behavior Disorder (RBD) is a
parasomnia that occurs in the state of sleep called REM. REM is most commonly
known as the state of sleep where one is dreaming and gets its name from the eyes
rapidly moving horizontally back and forth while dreaming. This state has also
been called paradoxical sleep because the brain is just as active as it is
during wake (however, the story is a bit more complicated because research has
shown that dreams can also occur during non-REM sleep, but they usually occur
during REM sleep). Most people spend about 25% of their night in REM sleep. During
this state of sleep, your brain sends signals from your lower brainstem to
inhibit motor signals so that you do not physically act out your dreams. This
inhibition is clinically called muscle atonia. For those with RBD, this
inhibition does not occur, and therefore, the body is able to act out its
dreams. Loss of muscle atonia during REM
sleep is the primary indicator of this disorder and is easily diagnosed during
an all-night sleep polysomnogram.
The people that find themselves in the clinic for this
disorder tend to do so because of acting out violent behavior while dreaming.
People have reported being chased or attacked then only to awaken while
assaulting their bed partner. There is no evidence why acting out aggressive
dreams is more common in this disorder, but it could just be that one is more
likely to seek help when they are putting themselves or their bed partners at
risk. This disorder tends to be more prevalent in older males (60yr+), and it's
estimated that about 0.5% of the population has RBD. RBD can be classified as either
primary or secondary disorder, with the estimates from 38-64% of patients with
primary RBD going on to develop a neurodegenerative disorder within 15 years,
such as Parkinson’s Disease (PD). However, only a minority of patients with PD
begin with RBD. It has been speculated that those with RBD, who later develop
PD, could be a distinct subgroup. Secondary RBD has been associated with
Narcolepsy. Pharmacological agents, such as tricylic antidepressants, SSRIs
(fluoxetine, paroxetine, citalopram, sertraline, and venlafacine), alcohol, and
beta blockers have also all been associated with secondary RBD. Clonazepam is
an effective treatment of RBD for 90% of sufferers.
How does the research
that you are involved with begin to recognize some of the connections between
sleep and mental health?
Disruption in sleep and circadian rhythms is one of the most
prevalent symptoms of psychiatric disorders. We now have decades of studies
comparing healthy controls with those suffering from a psychiatric disorder. I
will just touch on a few historical findings, as well as some more recent
studies that show a connection between sleep and mental health.
It has been known for some time now that people suffering
from major depressive disorder (MDD) show a decrease in slow wave sleep (this
is the deepest stage of sleep and is known as stage 3). They also experience
their first REM period earlier and this period lasts longer than healthy
controls. This correlation, of an earlier and longer first REM sleep period,
has been shown to persist after remission and can even precede a depressive
episode. Some researchers have suggested that this can serve as a biological
marker for MDD. One of the ways to increase the duration and depth slow wave
sleep (SWS) in this first sleep cycle, which precedes REM, is through sleep
deprivation. Sleep deprivation has been found to act as an antidepressant in
that subjective reports of depressive symptoms seem to disappear when the
patient is sleep deprived. However, they quickly return once the patient goes to
sleep; and, for those with bipolar disorder, sleep deprivation can trigger a
manic episode. Many, but not all, antidepressants inhibit REM sleep. This is
another interesting finding that indicates there is an intimate relationship
between mental health and sleep. Although, despite decades of research, much of
this relationship is still a mystery, as is most of the functioning of the
brain.
A fairly recent finding in our lab, looks at differences in
sleep spindles, is a burst of oscillatory brain activity visible on an EEG,
between people with schizophrenia and healthy controls. Sleep spindles occur during
stage 2 of sleep. What we found is a reduction in spindle number and duration
in people with schizophrenia. The area of the brain that generates sleep
spindles has also been indicated in working memory, language, and sensorimotor
integration. It is also the area of the brain where sensory input can be
reduced or enhanced on the way to the brain. Deficits in both attention and
sensory motor gating are common in people with schizophrenia.
One of the most interesting findings coming from our lab
recently was that rats can have areas of their brain that are actively sleeping
while the animal is awake for all practical purposes. Many species of birds and
marine mammals can have one half of their brain sleeping while the other half
is awake (unihemispheric slow wave sleep). In rats it was assumed that they
were either asleep or awake. Although they don't sleep with half their brain,
areas of the brain can be going off-line and into sleep while the animal still
appears actively awake. This has also been found in humans and, in fact, parts
of your brain involved in memory can begin to "sleep" up to 20min
before you experience subjective sleep. Perhaps this is one of the reasons
while someone who is awake for 24hrs is just as impaired as someone who is
legally drunk. Another reason not to sleep and drive.
As we further explore the reciprocal relationship between
waking and sleeping brain states, perhaps we will one day be able to more
accurately diagnose, treat, and perhaps even prevent the number of people that
suffer from mental health disorders.
I know that
meditation is a passion of yours and that some of the research that you are
involved with is looking at meditation. What can you share about the power of
meditation and your experiences with meditation?
I started meditating about 8yrs ago and have been meditating
daily for about 5yrs now. Hands down, it
has been the most effective way of reducing daily stress and increasing my
general quality of life that I have come across. It has also been the most challenging
practice I have ever engaged in. Knowing the science behind it helps me
understand why all of these apply.
In the broadest
sense, meditation is the act of directing your attention back, again and again,
to an object or state of being that one chooses and holding it there. This is
opposed to the hundreds of times a day that our mind free associates and gets
lost in its own self reflective thoughts of I, me, and mine. This free
association is our default state and is what the brain has been found to be
doing at rest. When the brain is imaged using fMRI during rest, the part of the
brain that is most active has been coined the Default Mode Network (DMN). There
is nothing wrong with the mind's active meanderings, but with so many things
clamoring for our attention these days, and probably nothing yells louder than
our own self-reflective thoughts, it's nice to put the mind at rest once and a
while and, paradoxically, I have found that paying attention is both relaxing
and rejuvenating. It has also helped me to realize that my thoughts are not who
I am and to be able to treat them with a degree of curiosity and amusement that
they deserve.
One of the reasons
meditation can be so challenging in the beginning is because one is literally
rewiring their brain to behave in a different way. Through years of not paying
attention to how we use our minds, the path of least resistance is to mind
wander. Some people struggle with this more than others, but I wasn't even
aware to the extent that this was the case, until I actively decided to
"watch" what my mind did when I was trying to do something as simple
as count my breath for 35min. At first I was generally surprised at how
difficult it was, but, over time, it became easier and easier. It is quite
amazing at how much basic richness in experiencing the present moment is
available when I let my thoughts settle, so that I can be more present to my
experience vs. my thoughts about my experience.
Meditation research has been going on since the 1960's;
however, based upon the number of publications, it has continued to increase
greatly over the last 15yrs or so. Our lab, in collaboration with Center of
Investigating Healthy Minds (CIHM), has been investigating the
neurophysiological correlates of meditation for a number of years now. Previous
studies of long term meditators (LTMs) vs. healthy controls have found the
following: greater tolerance for pain, increased volume in the hippocampus
(area involved in memory), less motor deficits after sleep restriction, more robust immune response, various positive
psychological effects (increased subjective well-being, reduced psychological
symptoms and emotional reactivity, and improved behavioral regulation),
reduction in morning stress hormones, and enhanced brain connectivity just to
name some. Some of these effects have been found in even short meditation
training sessions over a period of 8weeks. The current meditation study we are
working on is systematically comparing LTMS, with those learning Mindfulness Based
Stress Reduction (MBSR), a control group similar to MBSR (but without the
meditation) and a wait list control in areas such as: brain activity during
sleep, brain imaging during emotional tasks in an MRI machine, markers for
stress, prosocial emotional states as well as measuring psychological and
physical reactions to a stressor. Through these studies, we hope to show that
even 8weeks of training can show significant changes in these markers and help
to better understand how meditation training affects numerous psychological and
physiological states of being.
Anything else that
you would like to say?
One area of sleep I just want to briefly mention since it is
becoming more and more prevalent as the number of obese people in the U.S. rise,
is obstructive sleep apnea (OSA). I have seen many people in the lab who stop
breathing anywhere from 10 times per hr to 100+ per hr. Each time this occurs,
oxygen supply is cut off to the body and brain and in some ways can resemble a
mini-stroke. Many people with OSA complain of feeling unrested after awakening,
memory problems, and daytime sleepiness. A recent study at UW-Madison found
that people with severe sleep disordered breathing have a 5 fold increase of
dying of cancer, and even those with mild OSA double their chances. There have
also been numerous studies showing increase risk for cardiovascular disease in
those untreated. It is estimated that 1 in 5 Americans suffer from some form of
sleep disordered breathing. If you are
interested in more info on sleep and basic steps for good sleep hygiene, here
is the link to Wisconsin Sleeps website:
http://wisconsinsleep.org/index.html
There is even a short quiz to determine your risk of OSA.
Thanks Rick for your insights on sleep, sleep disorders, and it's impacts on health and wellness.
Jeff Ryan, LPCIT, CSAC
Therapist
Get Connected Counseling
